The term onychopathy encompasses a broad range of medical conditions that affect the nails, including both physical and functional disorders. It is a comprehensive term that describes any disease or condition that impacts the structure and health of the nails, which can be caused by various factors such as infections, systemic diseases, trauma, or nutritional deficiencies. Understanding onychopathy is essential for accurate diagnosis and treatment, as it can provide insights into an individual's overall health and well-being.
What You'll Learn
- Onychomycosis: Fungal infections causing nail thickening, yellowing, and brittleness
- Psoriasis: Autoimmune disorder leading to scaly, red patches on skin and nails
- Onychogryposis: Genetic condition affecting nail growth, often with deformities
- Acrodermatitis: Inflammatory condition causing nail and skin changes
- Onchocerciasis: Parasitic infection causing skin and eye irritation, nail changes

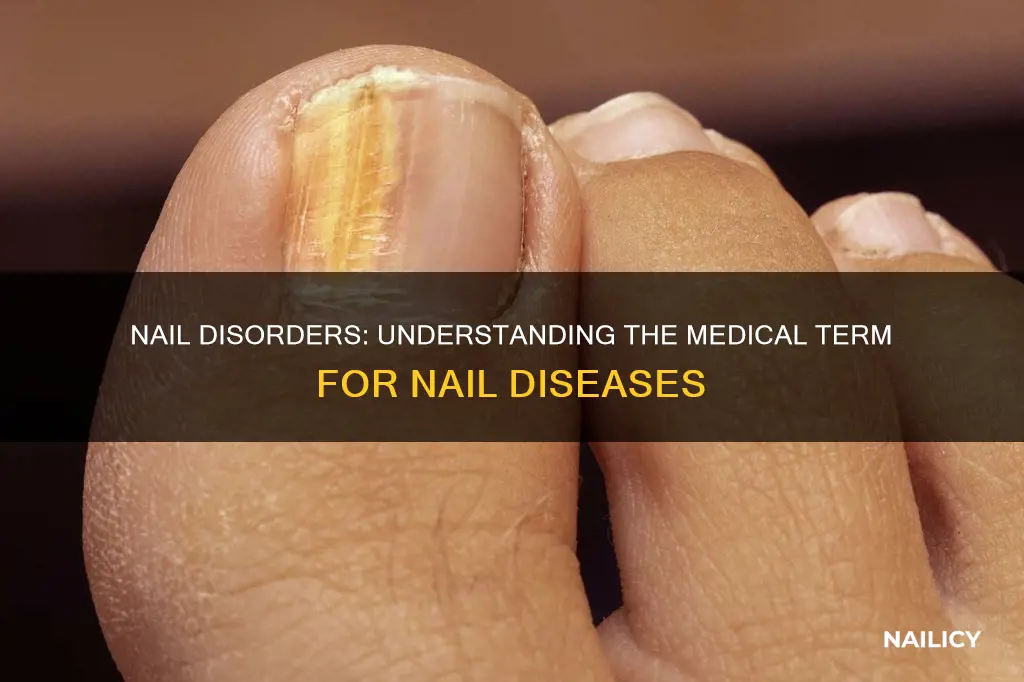
Onychomycosis: Fungal infections causing nail thickening, yellowing, and brittleness
Onychomycosis is a common term used to describe a group of fungal infections that primarily affect the nails. These infections are caused by various types of fungi, including dermatophytes, yeasts, and molds. Onychomycosis can lead to several symptoms, with the most noticeable being nail thickening, yellowing, and brittleness. The condition often starts as a small, discolored area on the nail, which may initially go unnoticed. Over time, the affected nail can become thickened, distorted, and separated from the nail bed. This progression can significantly impact a person's quality of life, affecting their physical appearance and even causing discomfort or pain.
The fungi responsible for onychomycosis thrive in warm, moist environments, making the condition more prevalent in areas with high humidity or in individuals with frequent exposure to such environments, such as swimmers or those living in tropical regions. Common risk factors include a weakened immune system, certain medications, and prolonged use of antibiotics or corticosteroids. Individuals with diabetes, arthritis, or circulatory issues are also more susceptible.
Diagnosing onychomycosis typically involves a visual examination of the nail, but a doctor may also take a small sample of the nail for laboratory testing to confirm the presence of fungi. Treatment options vary depending on the severity and type of infection. Mild cases may respond to over-the-counter antifungal creams or oral medications. More severe infections might require stronger antifungal treatments, including oral antifungal drugs or, in extreme cases, surgical removal of the affected nail.
Prevention is key to managing onychomycosis. Maintaining good foot hygiene, keeping nails short and clean, and using antifungal foot powders can help reduce the risk of infection. Wearing sandals in public showers or pools can also prevent exposure to fungi. For those with existing onychomycosis, regular nail care and prompt treatment of any new infections are essential to prevent the condition from worsening.
In summary, onychomycosis is a fungal infection that can lead to significant changes in nail appearance and texture. Early diagnosis and treatment are crucial to managing the condition effectively and preventing further complications. With proper care and attention, individuals with onychomycosis can maintain healthy nails and overall well-being.
Unraveling the Mystery: Pinkie Nails and Hispanic Culture
You may want to see also

Psoriasis: Autoimmune disorder leading to scaly, red patches on skin and nails
Psoriasis is an autoimmune disorder that primarily affects the skin and nails, causing a variety of symptoms that can be both uncomfortable and aesthetically concerning. It is a chronic condition, meaning it persists over a long period, often with periods of flare-ups and remission. This disease occurs when the immune system mistakenly attacks the body's own healthy cells, leading to an accelerated growth cycle of skin cells. As a result, the skin cells build up rapidly, forming thick, scaly patches that are often red and inflamed. These patches, known as plaques, are typically found on the elbows, knees, scalp, lower back, and nails, but they can appear anywhere on the body.
The exact cause of psoriasis is not fully understood, but it is believed to be a combination of genetic and environmental factors. People with a family history of psoriasis are at a higher risk of developing the condition. Triggers such as stress, certain medications, infections, and even weather changes can also contribute to flare-ups. The immune system's role in psoriasis is crucial; it stimulates the rapid production of skin cells, leading to the characteristic symptoms.
In terms of nail involvement, psoriasis can affect the nails in various ways. It can cause pitting, where small, depressed areas form on the nail surface, resembling the surface of a golf ball. This is often an early sign of nail psoriasis. The nails may also become thickened, discolored, and brittle, sometimes separating from the nail bed, a condition known as onycholysis. In severe cases, psoriasis can lead to the nail becoming distorted and even result in the nail falling off.
Treating psoriasis often involves a multidisciplinary approach, including dermatologists, rheumatologists, and other specialists. The goal is to control the symptoms, reduce inflammation, and prevent flare-ups. Common treatments include topical medications, light therapy, and systemic medications. Biologics, a newer class of drugs, have shown significant promise in treating moderate to severe psoriasis by targeting specific immune system molecules.
Living with psoriasis can be challenging, but with proper management and support, many people can lead fulfilling lives. It is essential to work closely with healthcare professionals to develop a personalized treatment plan and to address any psychological impacts that may arise from living with a visible condition. Understanding the condition and its treatment options empowers individuals to take control of their health and improve their quality of life.
Unraveling the Mystery: What Does 'Nail' Really Mean?
You may want to see also

Onychogryposis: Genetic condition affecting nail growth, often with deformities
Onychogryposis is a rare genetic disorder that primarily affects the growth and development of the nails. It is a condition that can lead to a variety of nail abnormalities, often resulting in deformities that can impact a person's quality of life. This condition is characterized by the abnormal growth and shape of the nails, which can vary in severity from person to person.
The term 'onychogryposis' itself is derived from the Greek words "onychos," meaning nail, and "gryposis," indicating a twisting or deformation. This name accurately describes the primary feature of the condition, which is the abnormal twisting or bending of the nails. Individuals with onychogryposis may experience a range of nail-related issues, including thickening, brittleness, and disfigurement. The nails can become curved, spoon-shaped, or even fused together, making them difficult to use and potentially causing pain and discomfort.
This genetic disorder is often associated with other systemic issues, as it is a part of a group of disorders known as 'nail-related disorders' or 'nail dystrophies.' These disorders can affect various parts of the body, including the skin, hair, and nails. Onychogryposis can be inherited in an autosomal dominant pattern, meaning that inheriting one copy of the mutated gene from one parent is sufficient to develop the condition. However, it can also occur spontaneously due to new mutations, especially in cases where there is no family history.
The causes of onychogryposis are not fully understood, but researchers believe that multiple genes are involved in the development of this condition. Mutations in these genes can disrupt the normal growth and differentiation of nail cells, leading to the observed deformities. Treatment options for onychogryposis are limited, and they often focus on managing the symptoms and improving the appearance of the nails. This may include the use of nail care products, protective footwear, and in some cases, surgical interventions to correct severe deformities.
In summary, onychogryposis is a genetic disorder that affects nail growth and results in various deformities. It is a rare condition that requires further research to understand its underlying causes and develop more effective treatment strategies. Early diagnosis and management can help individuals with onychogryposis cope with the physical and emotional challenges associated with nail abnormalities.
Understanding Onychorrhexis: The Medical Term for Nail Softening
You may want to see also

Acrodermatitis: Inflammatory condition causing nail and skin changes
Acrodermatitis is a term that encompasses a group of inflammatory conditions affecting the skin and nails. It is a descriptive term used to identify a range of disorders that primarily involve the upper extremities, particularly the hands and feet. This condition is characterized by a variety of symptoms, including redness, swelling, and changes in the appearance of the skin and nails. The term "acrodermatitis" is derived from the Greek words "akros," meaning "tip" or "end," and "dermatitis," which refers to inflammation of the skin. This name accurately reflects the localized nature of the condition, which primarily affects the distal parts of the limbs.
The clinical presentation of acrodermatitis can vary widely, making it a challenging diagnosis. Patients may experience symptoms such as erythema (redness), edema (swelling), and the development of nodules or plaques on the skin. In some cases, the condition can lead to the thickening and distortion of the nails, a process known as onycholysis. This nail involvement is a distinctive feature of acrodermatitis and can significantly impact a person's quality of life. The nails may become discolored, brittle, and prone to infection, requiring careful management and treatment.
There are several underlying causes and conditions associated with acrodermatitis. One of the most common causes is an autoimmune response, where the body's immune system mistakenly attacks its own tissues. This can lead to a variety of autoimmune diseases, including systemic lupus erythematosus (SLE) and rheumatoid arthritis. In some cases, acrodermatitis may be a manifestation of an underlying infection, such as a bacterial or fungal infection, which can trigger an inflammatory response. Additionally, certain medications and environmental factors can contribute to the development of this condition.
Diagnosing acrodermatitis requires a comprehensive approach, often involving a combination of clinical examination, laboratory tests, and imaging studies. A dermatologist or rheumatologist will carefully assess the patient's medical history, perform a physical examination, and may order blood tests to evaluate for autoimmune markers or infection. In some cases, a biopsy of the affected skin or nail may be necessary to confirm the diagnosis and rule out other conditions with similar presentations.
Treatment for acrodermatitis aims to reduce inflammation, manage symptoms, and prevent complications. This may include the use of corticosteroids to reduce swelling and redness, immunosuppressive medications to modulate the immune response, and antifungal or antibiotic treatments for underlying infections. In severe cases, physical therapy or occupational therapy can help patients manage nail deformities and improve their overall function. Early diagnosis and treatment are crucial to prevent long-term complications and ensure the best possible outcome for individuals affected by this inflammatory condition.
Unraveling the Mystery: What Light Blue Nails Say About a Girl
You may want to see also

Onchocerciasis: Parasitic infection causing skin and eye irritation, nail changes
Onchocerciasis, also known as river blindness, is a parasitic infection caused by the filarial worm Onchocerca volvulus. This disease is prevalent in tropical and subtropical regions, particularly in Africa, South America, and parts of the Middle East. While it primarily affects the skin and eyes, it can also lead to various complications, including changes in the nails. Understanding onchocerciasis and its impact on nail health is essential for early detection and management.
The parasitic infection can cause significant skin irritation and rashes, which are often the first noticeable symptoms. These skin manifestations are a result of the immune response to the worm's presence and the release of inflammatory substances. Over time, the skin may become thickened, rough, and discolored, especially in areas where the worm is most active, such as the face, neck, and limbs. The skin changes can be quite distressing and may lead to social stigma and psychological distress for affected individuals.
In addition to skin irritation, onchocerciasis can also affect the eyes, a condition known as onchocerciasis ophthalmica. The parasites can migrate to the eyes, causing inflammation and damage to the optic nerve and retina. This can result in vision problems, including blurred vision, eye pain, and even blindness in severe cases. Eye involvement is a major concern as it can lead to permanent vision loss if left untreated.
Nail changes are another significant manifestation of onchocerciasis. The infection can cause various nail abnormalities, such as onycholysis (separation of the nail from the nail bed), dystrophy (nail thickening and deformity), and hyperkeratosis (excessive thickening of the skin at the nail's base). These nail changes are often a result of the chronic inflammation and irritation caused by the parasitic infection. The nails may become discolored, brittle, and prone to infections, further complicating the overall health of the individual.
Managing onchocerciasis involves a combination of treatments. Anthelmintic drugs are used to kill the parasitic worms, reducing their numbers and alleviating symptoms. In addition, topical and oral anti-inflammatory medications can help manage skin irritation and eye inflammation. For nail changes, proper hygiene and regular nail care are essential. Keeping the nails clean and trimmed can prevent infections and promote better overall nail health. In severe cases, surgical intervention may be required to address nail deformities.
Early diagnosis and treatment of onchocerciasis are crucial to prevent long-term complications. Individuals living in endemic areas should be educated about the disease, its symptoms, and the importance of seeking medical attention. With proper management and support, those affected by this parasitic infection can improve their quality of life and reduce the impact of skin, eye, and nail-related complications.
Mastering the Art of 'Nailed It': Unlocking Success Secrets
You may want to see also
Frequently asked questions
The term you are looking for is "onychopathy" or "nail disease." It encompasses a wide range of medical conditions that impact the health and appearance of the nails.
Yes, several factors can contribute to nail disorders. These include fungal infections, trauma to the nail, nutritional deficiencies, autoimmune diseases, and certain medications. For example, onychomycosis is a fungal infection that can cause discolored and thickened nails.
A fungal nail infection often presents with yellow or white discolored nails, thickening, brittleness, and sometimes a foul odor. It is usually slow-progressing and may spread to other nails. In contrast, a nail injury, such as a bruise or a broken nail, typically causes immediate pain, swelling, and visible damage to the nail plate.
While some nail conditions are unavoidable, certain measures can help prevent or manage them. Maintaining good foot hygiene, keeping nails clean and trimmed, wearing protective footwear to prevent trauma, and ensuring a balanced diet with adequate nutrients can all contribute to nail health.
Treatment options vary depending on the specific condition. For fungal nail infections, antifungal medications, topical treatments, or oral antifungals may be prescribed. In cases of trauma or injury, rest, proper nail care, and in some cases, surgical intervention might be required. For nutritional deficiencies, addressing the underlying cause and supplementing the necessary nutrients can help improve nail health.







