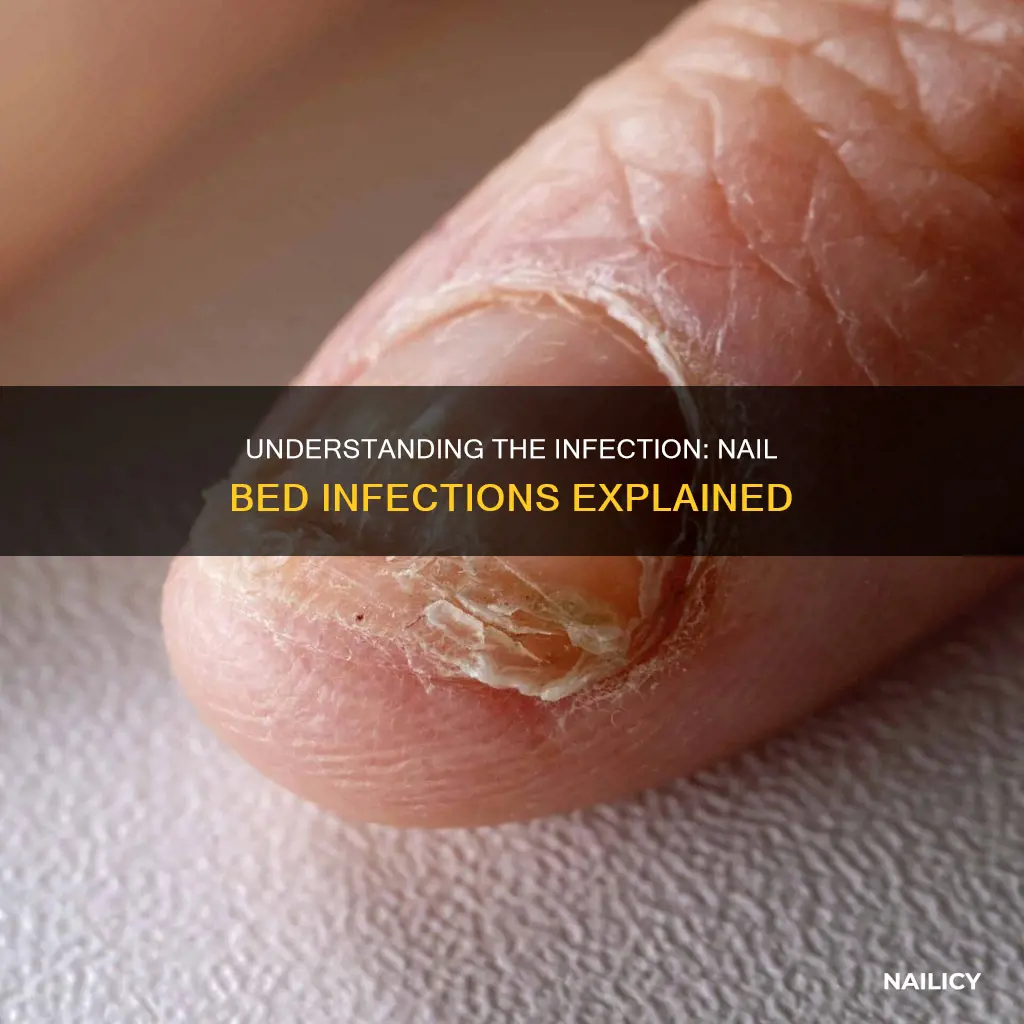
Infections along the fingernails, also known as paronychia, are common medical conditions that can cause significant discomfort and pain. These infections typically occur when bacteria or fungi enter the skin around the nail, often through small cuts or injuries. Paronychia can be acute, appearing suddenly and causing redness, swelling, and sometimes drainage, or it can be chronic, recurring over time and often associated with underlying conditions like diabetes or weakened immune systems. Understanding the causes, symptoms, and treatment options for nail infections is essential for effective management and prevention.
What You'll Learn
- Onychomycosis: Fungal infection causing nail thickening, yellowing, and brittleness
- Paronychia: Inflammation of the skin around the nail, often painful and red
- Bacteria: Bacterial infections like Staphylococcus can cause nail bed infections
- Trauma: Injury to the nail or surrounding tissue can lead to infection
- Nail Bed Abscess: A painful, swollen, and red area under the nail due to bacterial infection

Onychomycosis: Fungal infection causing nail thickening, yellowing, and brittleness
Onychomycosis is a common fungal infection that primarily affects the nails, often starting with the toenails but also capable of impacting fingernails. This condition is caused by various types of fungi, including dermatophytes, yeasts, and molds. It is a prevalent issue, especially among older adults and individuals with weakened immune systems or conditions that affect the circulatory system. The infection can occur in any part of the nail, but it most commonly starts at the edge or tip, leading to changes in the nail's appearance and texture.
One of the most recognizable symptoms of onychomycosis is the thickening of the nail, which can become discolored and distorted. The affected nail may appear yellow, brown, or even white, with a thick, opaque appearance. As the infection progresses, the nail can become brittle, crumbly, and prone to breaking or lifting off the nail bed. In severe cases, the infection might spread to the surrounding skin, causing itching, redness, and inflammation.
The fungal infection can be challenging to treat, and its recurrence is common. It often spreads through direct contact with infected individuals, contaminated surfaces, or animals. Warm and humid environments, such as public showers, swimming pools, and locker rooms, provide ideal conditions for fungi to thrive and increase the risk of transmission. Poor hygiene, frequent exposure to moisture, and certain medical conditions can also contribute to the development of onychomycosis.
Treatment options for onychomycosis include antifungal medications, both topical and oral. Topical treatments are often used for mild to moderate cases and may include creams, ointments, or nail lacquers containing antifungal agents. More severe infections might require oral antifungal medications, which can be effective but may have side effects and require a longer treatment duration. In some cases, surgical intervention might be necessary to remove heavily infected nails, especially when the infection has caused significant damage to the nail bed or surrounding tissue.
Preventing onychomycosis involves maintaining good foot and nail hygiene, keeping the feet dry, and avoiding walking barefoot in public areas. Wearing sandals or flip-flops in shared showers and pools can reduce the risk of exposure. Additionally, individuals with a history of fungal infections or those at higher risk should consider regular foot inspections and consult a healthcare professional for personalized advice and treatment options. Early detection and treatment are crucial to managing this condition effectively and preventing its progression.
Nail Darkening: Understanding the Causes and When to Seek Help
You may want to see also

Paronychia: Inflammation of the skin around the nail, often painful and red
Paronychia is a common and often painful condition that affects the skin around the nail, particularly on the fingers. It is essentially an inflammation of the paronychium, the tissue that surrounds the nail. This condition can be acute or chronic, depending on the duration and severity of the symptoms. Acute paronychia is a sudden and intense inflammation, often causing redness, swelling, and pain around the affected nail. It typically develops rapidly and can be quite uncomfortable, making even the simplest tasks difficult.
The primary causes of paronychia are diverse and can include both bacterial and fungal infections. Bacterial infections, such as Staphylococcus aureus, are a frequent culprit, especially when the skin around the nail is damaged or broken. This damage can occur due to various factors like frequent nail biting, hangnails, or even trauma from tight rings or frequent hand washing. When the skin barrier is compromised, bacteria can easily invade and cause an infection, leading to paronychia.
Fungal infections, on the other hand, are another significant cause, especially in warm and humid environments. Fungi thrive in moist conditions, and when the skin around the nail becomes moist and warm, it creates an ideal breeding ground for these microorganisms. This type of paronychia often affects people with weakened immune systems or those who have had previous nail or skin infections.
Symptoms of paronychia can vary but typically include redness, swelling, and pain in the area around the nail. The affected area may feel warm to the touch and could even drain pus or clear fluid, indicating a bacterial infection. In more severe cases, the nail itself may become thickened, discolored, and brittle. If left untreated, paronychia can lead to chronic nail problems and even permanent nail damage.
Treatment for paronychia depends on the underlying cause. For bacterial infections, a course of antibiotics is often prescribed to clear the infection. Keeping the affected area clean and dry is essential, and applying warm compresses can help reduce swelling and pain. In cases of fungal paronychia, antifungal medications may be recommended, and maintaining good hygiene and dryness in the nail area is crucial. It is always advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Uncover the Mystery: What Are the White Things on Your Nails?
You may want to see also

Bacteria: Bacterial infections like Staphylococcus can cause nail bed infections
Bacterial infections, particularly those caused by Staphylococcus, can lead to a condition known as paronychia, which is an infection along the finger nail. This condition often starts as a small, painful bump or redness around the nail, but it can quickly progress if left untreated. Staphylococcus bacteria are commonly found on the skin and in the nose, and they can enter the nail bed through small cuts or injuries, leading to an infection. The bacteria multiply rapidly, causing inflammation, redness, and swelling in the affected area. In some cases, the infection may spread to the surrounding tissues, including the skin and soft tissues of the finger.
Paronychia can be acute or chronic, depending on the duration and severity of the infection. Acute paronychia is a sudden, short-term infection that often results from a minor injury, such as a hangnail or a cut around the nail. It typically causes redness, swelling, and pain in the area, and may even lead to the formation of a small, fluid-filled blister. If the infection is left untreated, it can progress to a chronic condition, which is more difficult to treat and may result in recurring symptoms.
Chronic paronychia is a persistent condition that can be caused by various factors, including repeated injuries, certain occupations (like cleaning or gardening), and underlying health issues. This type of infection often presents with persistent redness, thickening of the skin around the nail, and even permanent nail deformities. It may also be associated with symptoms like pain, sensitivity, and brittleness of the nail. Proper diagnosis and treatment are crucial to prevent the infection from worsening and to avoid long-term complications.
Treatment for bacterial nail bed infections typically involves a combination of approaches. Antibiotic medications, either in the form of oral pills or topical creams, are commonly prescribed to eliminate the bacterial infection. In more severe cases, a doctor might recommend a course of intravenous antibiotics to ensure the infection is completely eradicated. Additionally, keeping the nail clean and dry, applying warm compresses to reduce swelling, and avoiding activities that aggravate the condition are essential parts of the treatment plan.
Preventing bacterial nail bed infections is crucial, especially for individuals with a higher risk of developing such infections. Maintaining good personal hygiene, especially around the nails, is vital. This includes regularly trimming and filing the nails to prevent hangnails and cuts. Wearing gloves when engaging in activities that may cause nail injuries, such as gardening or household chores, can also reduce the risk. For those with chronic health conditions or weakened immune systems, it is essential to seek medical advice and follow proper wound care practices to minimize the chances of bacterial infections.
Unraveling the Mystery: What Do Nail Grooves Mean?
You may want to see also

Trauma: Injury to the nail or surrounding tissue can lead to infection
In the context of nail health, an infection along the fingernail is a serious concern and is often referred to as a 'nail bed infection' or 'nail infection'. This type of infection can occur when bacteria, fungi, or other microorganisms invade the nail bed and surrounding tissues. It is a common issue that can arise from various traumatic events or injuries to the nail or its surrounding areas.
Trauma to the nail or the surrounding tissue can create an entry point for pathogens, leading to an infection. This can happen due to several reasons, such as accidental injury, sports-related accidents, or even minor cuts and scrapes. For instance, if you accidentally knock your finger against a hard surface, the force can damage the nail and create a small wound. This wound, even if minor, provides an opportunity for bacteria to enter and potentially cause an infection. Similarly, sports injuries, such as those sustained during contact sports or accidents involving sharp objects, can also lead to nail and tissue trauma, increasing the risk of infection.
The human body has natural defenses to fight off infections, but when the nail and surrounding tissues are damaged, these protective mechanisms may be compromised. As a result, bacteria or fungi can multiply rapidly, leading to symptoms such as redness, swelling, pain, and sometimes discharge around the nail. In more severe cases, the infection can spread to the bloodstream, causing systemic symptoms like fever and chills.
It is crucial to address nail and tissue trauma promptly to prevent the development of a full-blown infection. Simple measures like cleaning the wound with soap and water, applying antiseptic ointment, and covering the injury with a sterile bandage can help reduce the risk of infection. Seeking medical attention for deep or persistent wounds is essential to ensure proper treatment and prevent complications.
In summary, trauma to the nail or surrounding tissue can have serious consequences, potentially leading to infections that require medical attention. Understanding the risks and taking appropriate precautions can help individuals maintain good nail health and prevent complications associated with nail bed infections.
The Painful Reality of a Broken Fingernail: What to Expect
You may want to see also

Nail Bed Abscess: A painful, swollen, and red area under the nail due to bacterial infection
A nail bed abscess is a painful and often concerning condition that occurs when a bacterial infection develops under the nail. This infection can be a result of various factors, including poor hygiene, trauma to the nail, or underlying health conditions that compromise the immune system. The affected area becomes swollen, red, and tender, making it difficult to ignore. It is essential to understand the causes and symptoms to seek appropriate treatment and prevent further complications.
When a bacterial infection sets in, it can lead to the accumulation of pus and fluid beneath the nail plate. This pus is a collection of dead tissue, bacteria, and white blood cells, which the body's immune system is trying to fight off. The infection may start as a small, localized redness and swelling but can quickly progress, causing the nail to become discolored and distorted. In some cases, the abscess can drain on its own, but this is often accompanied by intense pain and discomfort.
Identifying the symptoms of a nail bed abscess is crucial for early intervention. The affected area will typically be warm to the touch and may have a distinct, unpleasant odor due to the bacterial activity. As the infection progresses, the redness may spread, and the nail may become thickened and discolored. In severe cases, the surrounding skin can become infected, leading to a more extensive and painful condition. It is important to note that nail bed abscesses can affect any nail but are most commonly observed on the toes due to their exposure to potential trauma and moisture.
Treating a nail bed abscess requires prompt medical attention. The primary goal is to drain the pus and remove the source of the infection. This often involves a minor surgical procedure where a small incision is made to allow the pus to drain. Antibiotic medications may also be prescribed to eliminate the bacteria and prevent further spread. Proper hygiene is essential during the healing process, including keeping the nail and surrounding area clean and dry.
In addition to medical treatment, there are several self-care measures that can aid in recovery. Elevating the affected limb can help reduce swelling, and applying warm compresses may encourage the abscess to drain naturally. Over-the-counter pain relievers can provide temporary relief from discomfort. However, it is crucial to avoid any attempt to pop or squeeze the abscess, as this can lead to further complications and potential scarring. Seeking professional medical advice is essential to ensure proper diagnosis, treatment, and guidance throughout the recovery process.
Unraveling the Mystery: What Do Ridges in Your Nails Indicate?
You may want to see also
Frequently asked questions
An infection along a finger nail is commonly referred to as a paronychia. This condition occurs when the skin around the nail becomes inflamed and infected, often due to bacteria or fungi. Paronychia can be acute or chronic, and it may affect one or multiple nails.
Paronychia can have several causes, including trauma to the nail, such as repeated tapping or biting, which can introduce bacteria or fungi under the nail. Other factors include nail injuries, cuts, or hangnails, as well as certain medical conditions like diabetes or autoimmune disorders that weaken the immune system.
Treatment for paronychia depends on the severity and underlying cause. Mild cases may respond to home remedies like keeping the nail clean and dry, applying warm compresses, and using over-the-counter antifungal or antibacterial ointments. More severe infections may require medical attention, including prescription antibiotics or antifungal medications, and in some cases, surgical drainage to relieve pressure and promote healing.







