Nail psoriasis is a condition that affects the nails, often occurring alongside the skin and joint symptoms of psoriasis. It can cause a range of changes to the nails, including thickening, yellowing, pitting, and even separation from the nail bed. This condition can be a source of significant distress and disability, impacting a person's appearance and functionality. Understanding the causes, symptoms, and treatment options for nail psoriasis is crucial for effective management and improved quality of life.
| Characteristics | Values |
|---|---|
| Definition | Nail psoriasis is a condition where the immune system mistakenly attacks the skin cells on the nails, leading to inflammation, thickening, and deformity of the nails. |
| Symptoms | - Nail pitting - Separated or loose nails - Discolored nails - Thickened nails - Brittle nails - Deformed nails (e.g., spoon-shaped or crescent-shaped) |
| Causes | - Genetic predisposition - Autoimmune response - Environmental triggers (e.g., stress, injury, infection) |
| Risk Factors | - Family history of psoriasis - Psoriasis of the skin - Other autoimmune diseases - Stress and lifestyle factors |
| Complications | - Nail loss - Disfigurement - Difficulty in performing daily activities - Psychological impact |
| Treatment | - Topical treatments (e.g., corticosteroids, vitamin D analogs) - Oral medications (e.g., methotrexate, cyclosporine) - Biologics (e.g., etanercept, adalimumab) - Nail care and maintenance |
| Management | - Regular nail care - Protecting nails from injury - Stress management techniques - Healthy lifestyle choices |
| Prognosis | - Can vary - May improve with treatment - Long-term management is often required |
What You'll Learn
- Nail psoriasis: Inflammation causing pitting, thickening, and discolouration of nails
- Symptoms: Pain, swelling, and nail separation from the nail bed
- Treatment: Topical creams, oral medications, and light therapy
- Progression: Can lead to nail loss and deformity if untreated
- Management: Regular nail care and monitoring can help prevent complications

Nail psoriasis: Inflammation causing pitting, thickening, and discolouration of nails
Nail psoriasis is a condition that affects the nails, often a sign of an underlying inflammatory disease, typically associated with psoriasis. It can be a distressing and debilitating condition, impacting not only the appearance of the nails but also their function. This condition can cause a range of symptoms, with the most common being pitting, thickening, and discolouration of the nails. These symptoms can vary in severity and may affect one or multiple nails.
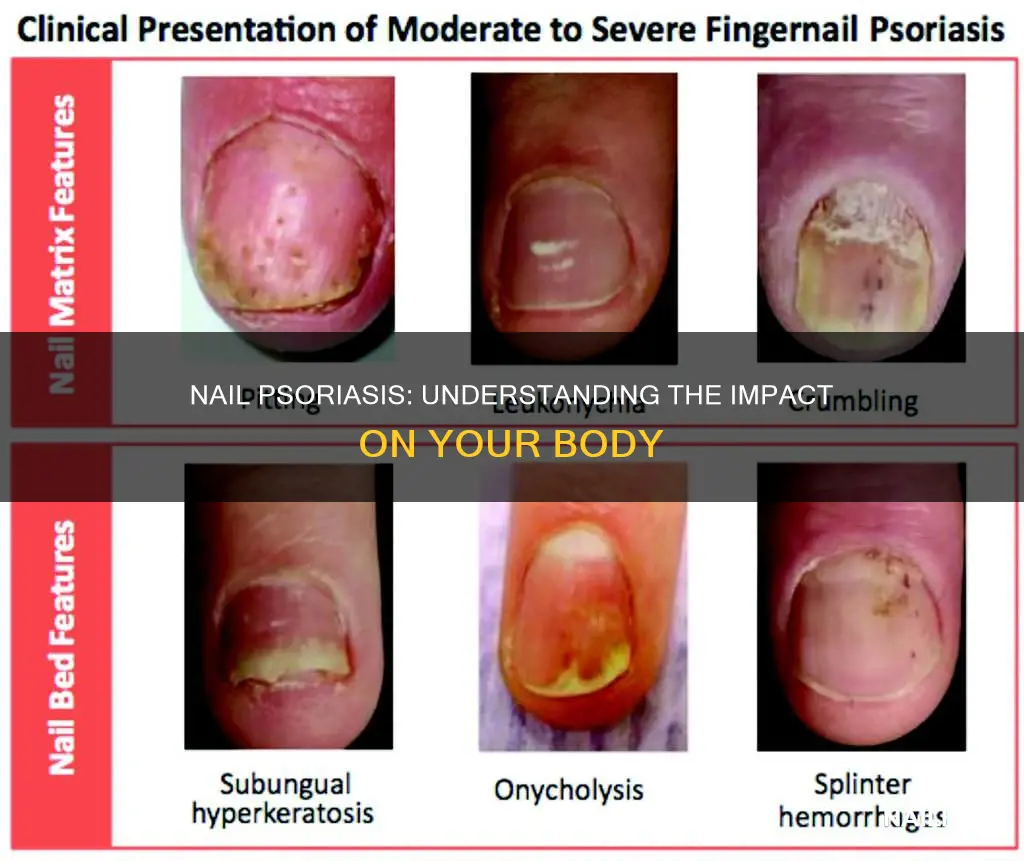
The pitting of the nails is a distinctive feature, presenting as small, round, or oval depressions on the nail surface. These pits can be shallow or deep and may be painful, especially when pressure is applied. Over time, the pits can become more pronounced and may even lead to the nail becoming fragile and prone to breaking or splitting. The thickening of the nails is another common issue, where the nail plate becomes abnormally thick, often causing discomfort and making daily activities challenging. This thickening can make it difficult to wear shoes or use tools that require a precise grip.
Discolouration of the nails is a result of the inflammation and can vary in appearance. The nails may turn a dull grey or brown, or in some cases, a bright red or purple. This discolouration is often a result of the buildup of dead skin cells and inflammation beneath the nail. The condition can also lead to the nails becoming brittle and fragile, making them more susceptible to damage and infection.
Nail psoriasis is a chronic condition, and its management often requires a multidisciplinary approach. Treatment options include topical medications, light therapy, and oral medications to reduce inflammation and slow down the progression of the disease. In some cases, surgery may be required to remove severely affected nails. Early diagnosis and treatment are essential to prevent further nail damage and to manage the associated pain and disability.
Living with nail psoriasis can be challenging, but with the right support and treatment, many people can lead a fulfilling life. It is important to seek medical advice if you suspect you have this condition, as early intervention can significantly improve long-term outcomes. Understanding the symptoms and seeking appropriate treatment can help individuals manage the condition effectively and maintain the health of their nails.
Unraveling the Mystery: Flash Cure's Impact on Nail Health
You may want to see also

Symptoms: Pain, swelling, and nail separation from the nail bed
Nail psoriasis is a condition that affects the nails, often an extension of the skin and joint inflammation associated with psoriasis. It can cause significant discomfort and impact a person's quality of life. One of the most common and noticeable symptoms is the pain, swelling, and separation of the nails from their underlying nail bed. This condition can affect any or all of the nails, including the toes and fingers.
When a person has nail psoriasis, the nails may become thickened, discolored, and prone to flaking or crumbling. The pain is often described as a throbbing or burning sensation, which can be exacerbated by movement or pressure. This pain can radiate to the surrounding areas, such as the fingertips or the joints, making even simple tasks like buttoning a shirt or gripping objects difficult.
The swelling associated with nail psoriasis is typically noticed around the nail matrix, the area where the nail grows from the cuticle. This swelling can lead to a visible distortion of the nail shape, making it appear misshapen or uneven. In some cases, the nail may lift or separate from the nail bed, creating a gap that can trap dirt and debris, leading to further infection and discomfort.
Nail separation from the nail bed, known as onycholysis, is a serious symptom that can have multiple causes. In the context of psoriasis, this separation can occur due to the inflammation and damage caused by the disease. The nails may become loose and fragile, leading to easy peeling or even complete detachment from the nail bed. This can result in a painful condition where the nail bed is exposed, making it susceptible to infection and further complications.
Managing nail psoriasis often involves a combination of treatments aimed at reducing inflammation, promoting nail health, and alleviating symptoms. Topical treatments, such as corticosteroids or vitamin D3 analogs, can help reduce swelling and pain. In more severe cases, systemic medications or biologic therapies may be prescribed to control the underlying inflammation of psoriasis. Additionally, proper nail care, including gentle filing and regular cleaning, can help prevent infections and promote better nail health.
The Surprising Truth: Can Nails Be a Healthy Breakfast Choice?
You may want to see also

Treatment: Topical creams, oral medications, and light therapy
Nail psoriasis is a condition that affects the nails, often causing them to become thickened, discolored, and prone to pitting and separation from the nail bed. It is a form of psoriatic arthritis, an autoimmune disorder that can impact various parts of the body. This condition can be particularly distressing as it affects the appearance and functionality of the nails. The treatment of nail psoriasis aims to reduce inflammation, improve nail appearance, and prevent further damage. Here's an overview of the treatment options:
Topical Creams and Ointments: These are often the first line of treatment for nail psoriasis and are applied directly to the affected nails. Topical treatments can help reduce inflammation and slow down the progression of the disease. Corticosteroid creams are commonly prescribed to reduce swelling and redness. Calcineurin inhibitor creams, such as tacrolimus and pimecrolimus, are also used to suppress the immune response and reduce inflammation. These topical medications are typically applied several times a day, and the duration of treatment may vary depending on the severity of the condition. It is essential to follow the prescribed application guidelines and not exceed the recommended dosage.
Oral Medications: For more severe cases of nail psoriasis, oral medications may be necessary. These medications work systemically to reduce inflammation and control the immune response. One common oral treatment is methotrexate, an immunosuppressive drug that can help slow down the progression of psoriatic arthritis and improve nail symptoms. Other oral medications include cyclosporine and ustekinumab, which are used to manage moderate to severe cases. These medications may have potential side effects, so regular monitoring by a healthcare professional is crucial.
Light Therapy (Phototherapy): Phototherapy is a non-invasive treatment that uses controlled amounts of natural or artificial light to reduce inflammation and slow down the growth of psoriatic lesions. In the context of nail psoriasis, light therapy can be applied directly to the affected nails. This treatment is often used in conjunction with topical creams and oral medications to enhance their effectiveness. There are different types of light therapy, including ultraviolet A (UVA) and ultraviolet B (UVB) phototherapy. UVA light is particularly effective for nail psoriasis as it penetrates deeper into the skin and can help reduce inflammation and improve nail appearance. Phototherapy sessions are typically administered in a controlled environment by a healthcare professional, and the treatment plan is tailored to the individual's needs.
In addition to these treatments, lifestyle modifications can also help manage nail psoriasis. Maintaining a healthy diet, staying hydrated, and managing stress can contribute to overall well-being and potentially improve symptoms. It is crucial to work closely with a healthcare provider to determine the most suitable treatment plan, as the approach may vary depending on the severity and individual characteristics of the condition.
Ingrown Nails: Causes, Symptoms, and Treatment Options
You may want to see also

Progression: Can lead to nail loss and deformity if untreated
Nail psoriasis is a form of the autoimmune condition known as psoriasis, which primarily affects the skin but can also impact the nails. It occurs when the body's immune system mistakenly attacks the skin cells, leading to an overproduction of new skin cells. This rapid cell turnover can result in the thick, scaly, and discolored patches characteristic of psoriasis. When psoriasis affects the nails, it can cause a range of symptoms and complications, especially if left untreated.
The progression of nail psoriasis can vary in severity and may not always follow a linear path. Initially, the condition might present as small, white or yellow spots under the nail, often referred to as 'pitting' or 'oil drops.' These spots can grow and spread, leading to a more extensive involvement of the nail. As the disease advances, the nails may become thickened, discolored, and brittle. They can develop a rough, sandpaper-like texture and may even become separated from the nail bed, a condition known as 'onycholysis.' This can result in pain, sensitivity, and, in severe cases, the nail may even detach completely.
Over time, untreated nail psoriasis can lead to significant nail loss and deformity. The nails may become so damaged that they start to crumble or fall off, leaving behind a thin, fragile layer of skin. This can be particularly distressing and may impact an individual's quality of life, affecting their ability to perform daily tasks and maintain personal hygiene. In some cases, the nail bed may also be affected, leading to permanent damage and changes in the nail's structure.
The progression of nail psoriasis is often influenced by various factors, including the individual's overall health, the severity of their psoriasis, and the effectiveness of their treatment. Certain triggers, such as stress, infections, or specific medications, can also accelerate the condition's advancement. It is crucial for individuals with nail psoriasis to seek medical advice and develop a comprehensive treatment plan to manage their symptoms and prevent further complications.
Early intervention is key to managing nail psoriasis effectively. Treatment options may include topical medications, light therapy, oral medications, and biologic therapies, all aimed at reducing inflammation and slowing down the rapid cell turnover associated with psoriasis. Regular follow-ups with a dermatologist or healthcare provider are essential to monitor the condition's progression and adjust the treatment plan accordingly. With proper management, many individuals can experience significant improvement in their nail health and overall well-being.
Unraveling the Mystery: What's the Deal with a Yellow Big Toe Nail?
You may want to see also

Management: Regular nail care and monitoring can help prevent complications
Nail psoriasis is a condition that affects the nails, often occurring alongside other symptoms of psoriasis, an autoimmune disorder. It can cause a variety of changes to the nails, including thickening, pitting, discolouration, and separation from the nail bed. These symptoms can be not only aesthetically displeasing but also painful and potentially disabling. Effective management of nail psoriasis is crucial to prevent complications and maintain overall health.
Regular nail care is an essential part of managing nail psoriasis. This involves keeping the nails clean and well-maintained to reduce the risk of infection, which is a common complication in individuals with psoriasis. Start by gently cleaning the nails with a soft brush or a nail brush designed for sensitive skin. Warm water can help soften the nails, making them easier to clean. It's important to dry the nails thoroughly after washing to prevent moisture buildup, which can lead to fungal infections.
Nail care also includes proper trimming and filing. Use a nail clipper to trim the nails straight across, avoiding curved edges that can trap dirt and debris. Then, use a nail file to smooth any sharp edges and remove ridges. When filing, it's best to use a gentle, fine-grit file to prevent further irritation. Regularly filing the nails can help prevent the buildup of dead skin and reduce the risk of the nails becoming ingrown or infected.
Monitoring the nails is another critical aspect of management. Regularly inspect your nails for any changes or new symptoms. Look for signs of infection, such as redness, swelling, warmth, and drainage. If you notice any of these symptoms, seek medical attention promptly. Additionally, pay attention to any changes in nail texture, colour, or shape. For example, if your nails become thick and brittle, or if you notice white or yellow spots, these could be indicators of nail psoriasis or other underlying conditions.
By maintaining a consistent nail care routine and closely monitoring your nails, you can significantly reduce the risk of complications associated with nail psoriasis. This proactive approach can help prevent the progression of the condition and ensure that any issues are addressed early on, leading to better overall management of psoriasis. Remember, consistent care and attention to your nails can make a substantial difference in your quality of life.
Unraveling the Mystery: What Yellow Nail Beds Reveal About Your Health
You may want to see also
Frequently asked questions
Nail psoriasis is a condition that affects the nails, often occurring alongside other symptoms of psoriasis, an autoimmune disorder. It can cause changes in the appearance and function of the nails, which can be both physically and emotionally distressing.
While psoriasis typically affects the skin, nail psoriasis specifically targets the nails. It can lead to a variety of nail changes, including pitting, thickening, discolouration, and separation of the nail from the nail bed. These symptoms can vary in severity and may affect one or multiple nails.
Treating nail psoriasis often involves a combination of approaches. These may include topical treatments like corticosteroids or retinoids to reduce inflammation, oral medications to manage the underlying psoriasis, and specific nail care routines. In severe cases, procedures such as nail debridement or surgery might be recommended to remove severely affected nails and promote new nail growth.