When pus comes out of a nail, it is often a sign of an infection, typically caused by bacteria or fungi. This condition, known as paronychia, can occur around the nail bed or the side of the nail. It may be accompanied by redness, swelling, pain, and sometimes a foul-smelling discharge. The pus is a collection of white blood cells and dead tissue that the body produces to fight the infection. Seeking medical attention is crucial to determine the underlying cause and receive appropriate treatment, which may involve antibiotics or antifungal medications.
What You'll Learn
- Infection: Pus indicates a bacterial or fungal infection under the nail, often caused by trauma or poor hygiene
- Nail Bed Damage: Pus can result from injury to the nail bed, leading to inflammation and potential infection
- Acrokeratosis: This condition causes thick, scaly patches under the nails, sometimes accompanied by pus
- Onychomycosis: Fungal infections can cause nail thickening, discolouration, and pus formation
- Trauma and Injury: Physical damage to the nail can lead to pus accumulation, pain, and potential infection

Infection: Pus indicates a bacterial or fungal infection under the nail, often caused by trauma or poor hygiene
When pus comes out of your nail, it is a clear sign of an underlying infection. This condition, known as a subungual abscess or a nail bed infection, is often caused by a bacterial or fungal invasion. The presence of pus is a result of the body's immune response to the infection, as it tries to eliminate the harmful microorganisms. This can occur due to various factors, including trauma to the nail or surrounding area, poor hygiene, or even a weakened immune system.
In many cases, the infection starts as a minor issue, such as a small cut or injury near the nail. Over time, if left untreated, bacteria or fungi can enter the nail bed through this entry point, leading to an infection. The body's natural defense mechanisms then kick into action, resulting in the formation of pus as a means to contain and eliminate the pathogens. However, if the infection is not addressed promptly, it can spread and cause more severe complications.
Poor hygiene plays a significant role in the development of nail infections. Not keeping the nails clean and dry, especially in areas between the toes, can create a moist environment that is conducive to bacterial and fungal growth. Additionally, sharing personal items like towels or nail clippers can transfer infections from one person to another. It is crucial to maintain good hygiene practices to prevent the occurrence of pus-filled nail infections.
The symptoms of a nail infection often include redness, swelling, and pain around the affected area. The nail itself may become discolored, thick, and brittle. In severe cases, the infection can lead to the separation of the nail from the nail bed, causing the nail to lift or even fall off. If you notice any of these signs, it is essential to seek medical attention promptly to prevent further complications.
Treating a pus-filled nail infection typically involves a combination of medical interventions. Antibiotic or antifungal medications may be prescribed to target the underlying infection. In some cases, a minor surgical procedure might be required to drain the pus and remove any infected tissue. Proper nail care, including keeping the nails clean, dry, and trimmed, is also crucial during and after the treatment process. It is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Unraveling the Mystery: Pink Nails and Girl Power
You may want to see also

Nail Bed Damage: Pus can result from injury to the nail bed, leading to inflammation and potential infection
Nail bed injuries can be quite painful and often lead to complications, including the discharge of pus. When the delicate tissue under the nail, known as the nail bed, is damaged, it can become inflamed and infected, resulting in the accumulation of pus. This condition is not only unsightly but can also be a sign of an underlying issue that requires medical attention.
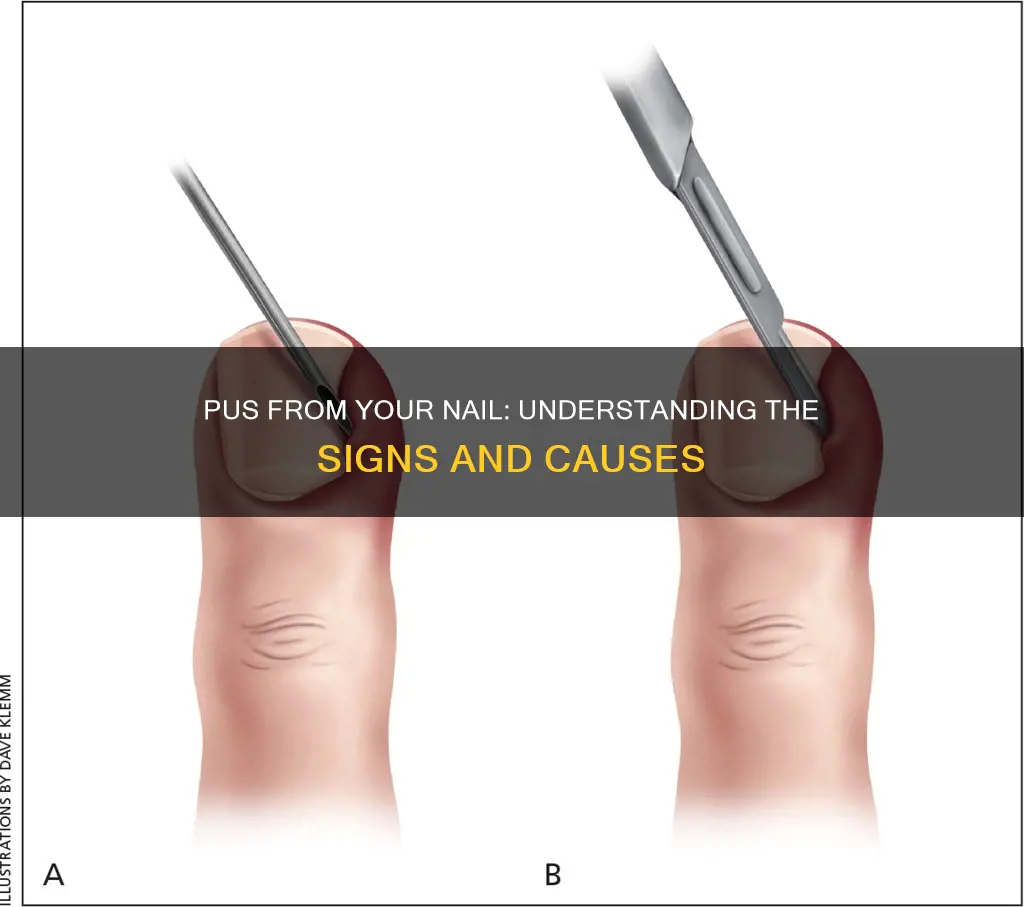
In many cases, nail bed injuries occur due to accidental trauma, such as dropping heavy objects on the nail or sustaining a blow to the hand. Even minor injuries can lead to significant problems if not treated promptly. The nail bed is rich in blood vessels, and any damage can cause bleeding, swelling, and eventually, the formation of a small pocket of pus. This pus is a result of the body's immune response to the injury, as white blood cells rush to the site to fight off potential infections.
Pus formation in the nail bed can be accompanied by other symptoms, such as redness, tenderness, and swelling around the affected area. The nail may also become discolored, taking on a yellow or dark hue. These signs indicate that the injury has progressed and may require immediate medical intervention. If left untreated, the infection can spread to the surrounding tissues and bones, leading to more severe complications.
Treating nail bed injuries and the resulting pus discharge is crucial to prevent further complications. The initial step is to clean the area gently with warm water and mild soap to reduce inflammation and remove any debris. Applying a topical antibiotic ointment can help prevent infection and promote healing. In some cases, a doctor may prescribe oral antibiotics to combat the infection more effectively. It is essential to keep the nail and surrounding area clean and dry to aid in the healing process.
In more severe cases, where the infection has spread or the nail bed is extensively damaged, medical procedures may be necessary. This could involve the removal of the affected nail or parts of the nail bed to allow for proper healing. Seeking prompt medical attention is vital to ensure the best outcome and prevent long-term damage to the nail and surrounding tissues. Proper care and timely treatment can help individuals recover from nail bed injuries and restore the health of their nails.
Unraveling the Mystery: Long Nails on Guys
You may want to see also

Acrokeratosis: This condition causes thick, scaly patches under the nails, sometimes accompanied by pus
Acrokeratosis, also known as keratoderma, is a rare skin condition that primarily affects the palms and soles of the feet, but it can also impact the nails. This condition is characterized by the thickening and hardening of the skin in these areas, often resulting in the formation of scaly patches. These patches can be quite persistent and may cause discomfort or pain, especially when they become inflamed or infected. One of the more concerning aspects of acrokeratosis is the potential for the development of pus-filled lesions.
When pus is present under the nails, it indicates an infection or inflammation that has progressed to a more severe stage. Pus is a byproduct of the body's immune response to infection, containing white blood cells, dead tissue, and bacteria or other pathogens. In the context of acrokeratosis, the pus may be a result of the skin's inability to regenerate normally, leading to the accumulation of dead skin cells and bacteria. This can create a vicious cycle where the infected area becomes more inflamed and painful, potentially requiring medical intervention.
The appearance of pus under the nails can be a sign of a bacterial infection, which may require antibiotic treatment. It is essential to seek medical advice if you notice this symptom, as it could indicate a more serious underlying condition. In some cases, the pus may be a result of a fungal infection, which can also affect the nails and skin. Proper diagnosis is crucial to determine the appropriate treatment, which may include antifungal medications or other interventions.
Managing acrokeratosis often involves a combination of topical and oral treatments. Topical medications, such as corticosteroids or retinoids, can help reduce inflammation and slow down the thickening of the skin. Oral medications, including vitamin A derivatives, may be prescribed to manage the condition more effectively. Maintaining good foot hygiene and keeping the skin clean and moisturized can also help prevent infections and manage symptoms.
In summary, acrokeratosis is a condition that can lead to thick, scaly patches under the nails, and the presence of pus may indicate a more severe infection or inflammation. Prompt medical attention is essential to receive an accurate diagnosis and appropriate treatment. With proper management, individuals with acrokeratosis can improve their quality of life and prevent further complications.
Unraveling the Mystery: What Your Nail Ridges Tell You
You may want to see also

Onychomycosis: Fungal infections can cause nail thickening, discolouration, and pus formation
Onychomycosis, a common fungal infection, can lead to a range of symptoms affecting the nails, including the formation of pus. This condition occurs when a fungus, often a type of dermatophyte, infects the nail bed and surrounding tissues. The infection can cause the nail to become thickened, discolored, and brittle, and in some cases, it may even lead to the discharge of pus.
When a nail is infected with a fungus, the infection can spread rapidly, especially if it goes untreated. The fungus thrives in warm, moist environments, making the nail bed an ideal breeding ground. As the infection progresses, it can cause the nail to thicken and become distorted in shape. This thickening is often a result of the fungus invading the nail matrix, the area where new nail cells are produced. Over time, the infected nail may change color, becoming yellow, brown, or even black, especially in the affected areas.
The presence of pus is a concerning sign of onychomycosis. Pus formation indicates an active bacterial infection, which is often a secondary complication of the fungal infection. Bacterial infections can occur when the fungal infection weakens the nail, making it more susceptible to bacterial invasion. The pus may be a result of the body's immune response to the infection, as it tries to eliminate the bacteria and protect the surrounding tissues.
Treating onychomycosis is crucial to prevent the infection from spreading and causing further damage. Treatment options typically involve antifungal medications, which can be administered orally or applied directly to the nail. In some cases, a combination of antifungal and antibacterial treatments may be required to address both the fungal and bacterial components of the infection. Early diagnosis and treatment are essential to manage the condition effectively and prevent long-term complications.
In summary, onychomycosis is a fungal infection that can lead to significant nail changes, including thickening, discolouration, and pus formation. The presence of pus indicates a bacterial infection, often a secondary complication. Prompt treatment with antifungal and, if necessary, antibacterial medications is crucial to manage the condition and prevent further nail damage.
Unraveling the Mystery: Red Nail Ring Finger Symbolism
You may want to see also

Trauma and Injury: Physical damage to the nail can lead to pus accumulation, pain, and potential infection
Physical trauma to the nail can result in a variety of issues, including the accumulation of pus, which is a clear sign of an infection. This often occurs when the nail bed or surrounding tissues are damaged, creating an entry point for bacteria. Common causes of such trauma include accidental injuries, such as dropping heavy objects on the foot or hand, or more specific incidents like sports-related accidents or even a simple cut or scratch. In some cases, repeated minor injuries can lead to chronic issues over time.
When a nail is injured, the body's natural response is to send white blood cells to the site to fight off any invading bacteria. This process can lead to inflammation and, in some cases, the formation of a small pocket of pus (abscess) beneath the nail. Pus is essentially a collection of dead white blood cells, bacteria, and tissue fluid, and its presence indicates an active infection. The body's immune response can cause the affected area to become swollen, red, and painful, often requiring immediate attention to prevent further complications.
In many cases, the initial injury might be minor, but the body's reaction can be significant. For instance, a small puncture wound caused by a nail or a sharp object can lead to an infection that, if left untreated, may result in the nail becoming separated from the nail bed, a condition known as onychomycosis or a nail abscess. This separation can cause the nail to become distorted and discolored, and the pus may drain through the nail, leading to a foul-smelling discharge.
Prompt treatment is crucial to manage the pain, prevent the spread of infection, and ensure the nail's health. Simple measures such as keeping the area clean and dry, applying warm compresses to reduce swelling, and using over-the-counter pain relievers can provide temporary relief. However, for more severe cases, medical intervention is necessary. A healthcare professional may prescribe antibiotics to clear the infection and, in some instances, may need to drain the abscess to remove the pus and dead tissue.
In summary, pus accumulation under or around the nail is a clear indicator of an infection, often resulting from physical trauma. Prompt recognition and treatment are essential to prevent the infection from spreading and to ensure the nail's proper healing. It is always advisable to seek medical advice for any persistent or severe symptoms to avoid potential complications.
Unraveling the Mystery: What Blue and White Nails Symbolize
You may want to see also
Frequently asked questions
Pus formation under a nail, known as a subungual abscess, is typically a result of a bacterial infection. This can occur when an injury or trauma to the nail bed leads to an infection, often caused by bacteria like Staphylococcus or Streptococcus. The body's immune response to the infection results in the accumulation of pus, which may drain through the nail.
Treatment for a subungual abscess involves draining the pus and addressing the underlying infection. This often requires a minor surgical procedure to create an incision and allow the pus to drain. Antibiotic medication may also be prescribed to eliminate the infection. In some cases, the affected nail may need to be removed to prevent further complications.
While some home remedies might provide temporary relief, it's crucial to seek medical attention for proper treatment. Keeping the area clean and dry, applying warm compresses, and using over-the-counter pain relievers can help manage symptoms. However, these methods do not address the infection and should not replace professional medical care.
Proper hygiene and injury prevention are key to reducing the risk of developing a subungual abscess. Avoid traumatic injuries to the nail bed, and ensure good foot or hand hygiene, especially if you have a pre-existing condition that makes you more susceptible to infections. If you notice any signs of infection, such as redness, swelling, or pain, seek medical advice promptly to prevent the condition from worsening.